Shoulder dislocations are a common presentation in the event environment – including OCR’s, aquatics, cycling and field events within athletics etc. Having treated hundreds of patients in this situation we decided to dedicate this weeks blog to all things shoulder dislocation.
 What is a shoulder dislocation?
What is a shoulder dislocation?
In simple terms, this is when the upper part of the arm (humerus) comes out of its socket (glenoid). There are 3 variations:
· Anterior – Where the head of the humerus is found in front of the socket (this occurs in 95% of cases)
· Posterior – Where the head of the humerus is found behind the socket (this occurs in 2-4% of cases).
· Inferior – Where the head of the humerus is sat below the socket (this occurs in < 0.5% of cases)
How do they occur?
For some people this is a regular occurrence due to an inherent laxity within the shoulder joint (ether from previous dislocations, hypermobility or due to unusual anatomy).
For these people simple movements such as elevating their arm can trigger a dislocation.
The majority of people however need a significant degree of traction (e.g. pulling someone over an obstacle) or force (e.g. fall from a bike) for the joint to dislocate.
Posterior dislocations are rare, but more likely to occur in those who have had a seizure or electric shock due to the way they land when they fall.
 What are the symptoms and signs?
What are the symptoms and signs?
· Shoulder pain – varies in intensity but can be severe
· Reduced range of arm movement – the patient will often brace their arm with their other hand to prevent it moving
· Shoulder asymmetry – the affected shoulder will look different to the other side.
What will the treating clinician do initially?
1) Administer pain relief
2) Check the pulses in the arm to ensure that a good blood flow is present
3) Check the sensation on the upper outer part of the arm to assess if the axillary nerve is affected
4) Feel the shoulder joint to feel for the head of the humerus and for any possible fractures.
 What pain relief options are used?
What pain relief options are used?
Inhaled quick acting medication is preferable, including:
· Entonox
· Penthrox
Intravenous medications can also be very effective however the risk of infection in a muddy environment needs acknowledging. They also often require greater monitoring and take longer to administer than inhaled preparations thus making them less favourable.
· Morphine
· Fentanyl
· Ketamine
· Paracetamol
· Midazolam
How is the shoulder relocated in the hospital setting?
There are a number of different techniques used which include:
· Traction – Counter Traction
· Scapular Manipulation
· Milch Technique
· FARES · SPASO
· Cunningham · Stimson
· Snowbird
· Kocher – no longer recommended due to complications
· Hippocratie – also no longer recommended.
 What about shoulder relocation in the event setting?
What about shoulder relocation in the event setting?
This is an area of fairly significant discussion.
Within the hospital setting it is common practice to take an x ray before performing any relocation manoeuvres to assess the type of dislocation and to check for any co-existing fractures. In the event world it is rare to have access to x-ray facilities without taking the patient to hospital.
Therefore a decision on whether to relocate the shoulder at the event or to transport the patient to hospital should be made. There are multiple factors to consider when making this decision:
Patient specific:
· How long will it take the patient to get to hospital by event ambulance?
· How well controlled is their pain?
· How busy is the local receiving hospital that day – i.e. how long will the patient need to wait for treatment?
· From the mechanism and examination, how likely is it that the dislocation is complicated by a fracture?
· Would having an x-ray affect how the shoulder is relocated? Event specific:
· If the patient goes by ambulance how long will the event be short of an ambulance for?
· If the event is busy and no ambulances are currently available, is there a space in the medical tent for this patient?
· Is there enough pain relief on site to keep the patient comfortable until they get to hospital?
NHS specific:
· If there were no event ambulances available, how long would it take an NHS ambulance to arrive?
· How will transferring this patient affect the local hospital in terms of workload in the context of it being a nominated receiving hospital and its business as usual priorities?
Taking everything into account it is usually more appropriate to try and relocate the dislocated shoulder in the event setting rather than taking the person to hospital.
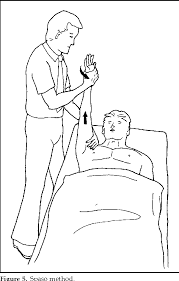 The RFU ICIS (Immediate Care in Sport) Course recommends using SPASO in the pre hospital setting as it is deemed to have a lower risk of complications if a co-existing fracture is present. To date we have used this method over 500 times successfully with no complications recorded.
The RFU ICIS (Immediate Care in Sport) Course recommends using SPASO in the pre hospital setting as it is deemed to have a lower risk of complications if a co-existing fracture is present. To date we have used this method over 500 times successfully with no complications recorded.
How easy is it to relocate?
In our experience > 97% of shoulders are relocated easily with a single attempt at the SPASO technique using entonox or penthrox as pain relief. The longer a patient waits for the procedure the greater the amount of muscle spasm that develops, making relocation more challenging and more painful for them.
Who can relocate shoulders?
· Some doctors: Those who have worked in A&E (or orthopaedics) are trained in this procedure however all doctors should also have additional pre – hospital training (e.g. ICIS course) before performing this procedure in the event setting.
· Some paramedics: The majority of paramedics are not trained in this procedure (as it is not part of NHS training) however some will undergo additional training in this area.
· More unusually other health care professionals (e.g. nurses, technicians) may also be trained to carry this out if they have done suitable additional pre hospital training.
What happens after the shoulder is relocated?
At this stage the shoulder will still be sore but will feel much more comfortable. It is helpful to give some basic pain relief (e.g. paracetamol) and place the patient in a broad arm sling.
Patients should then be advised to attend the local A&E department near home for a post reduction x-ray and follow up in fracture clinic.
How can I find out more on this topic?
Feel free to contact us at Contact Us and we will be happy to help answer your questions.


