Barely a week goes by without concussion making the sports headlines in one form or another. The upper levels of rugby have lead the way (in the UK) in concussion recognition and management, with numerous other sports following suit. But what about the event world – how well is concussion assessed and managed at mass participation events such as OCR’s or triathlons for example. Unfortunately its well know that beyond the level of elite sport, concussion is poorly diagnosed and therefore managed – leading to patients being put at risk.
Many of our SportsMedics team work in professional sport, so we have used our learning from the elite environment and translated it to the mass participation world. This helps us manage concussions that occur in a multitude of scenarios, from kicks in the head in a swim, to collisions in a cycle event and everything in between.
This blog looks at concussion in general and how an event medical team can put in place best practices in all sporting environments to manage it to correct way.
What is Concussion?
The NHS define concussion as “a temporary injury to the brain caused by a bump, blow or jolt to the head. It usually only lasts up to few days or weeks, although it sometimes needs emergency treatment and some people can have longer-lasting problems.”
Symptoms range widely and can include the following in varying degrees of severity:
· Headache
· Nausea or vomiting
· Amnesia (retro or anterograde)
· Dizziness
· Blurred vision
· Feeling not quite right
· Confusion
· Neck pain
· Sensitive to light
· Sensitive to noise
· Insomnia
· Sadness
· Nervous or anxious
· Irritability
· Fatigue/low energy
· Feeling slow
· Feeling like they are in a fog
· Off balance
The majority of concussions occur as a result contact to the head – and mostly with a surprisingly low velocity. However it is also possible to be concussed without direct head contact – e.g. in a whiplash type movement. It is also a common misconception that concussion can only occur following a loss of consciousness however this is not the case.
 How do you assess for it?
How do you assess for it?
The SCAT 5 is a standardized tool for assessing concussions, which takes around 10 – 15 minutes to perform and includes a symptom checklist, memory and balance tests. Ideally baselines are taken annually as a comparison however this is not compulsory and also rarely relevant in the mass participation event setting.
Any patient presenting to the medical team who could potentially have concussion should be assed using the SCAT 5, and equally anyone with a suspicious mechanism should be tested. It is not always apparent until performing the SCAT assessment that a person is concussed.
What is the GRTP?
The graduated return to play (GRTP) is the pathway to returning a patient with concussion back to physical activity.
This process involves a period of rest from all physical activity, followed by a structured return to sport over several stages. Depending on the severity of the symptoms it may be appropriate to restrict screen time and take time of work/education in the first few days – this is known as “brain rest”.
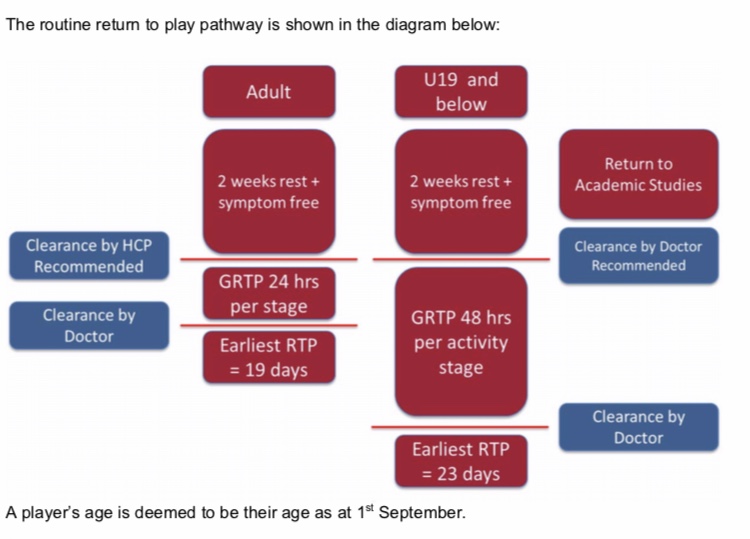
The exact GRTP varies from sport to sport, however the RFU have produced a version that can then be easily adapted for the physical activity type the patient usually partakes in. If there are no complications along the way then an adult patient may return to full sport on day 19-post injury, after clearance by a doctor. There will be 24 hours between each physical activity stage in this scenario.
 The basic GRTP is based on an adult patient with limited regular doctor contact – however the process can be amended for those who can see a doctor on a couple of occasions and have a baseline SCAT. In this scenario their earliest return to full sport will be 6 days if they are seen after the rest period and again at the end of the GRTP.
The basic GRTP is based on an adult patient with limited regular doctor contact – however the process can be amended for those who can see a doctor on a couple of occasions and have a baseline SCAT. In this scenario their earliest return to full sport will be 6 days if they are seen after the rest period and again at the end of the GRTP.
 The majority of patients make it through the GRTP with no issues at all and return to full sporting activity within the shortest allowed time, however others will take longer between each stage to get back to full activity. Those who remain symptomatic despite prolonged rest will require a review from a sports and exercise medicine consultant or a neurologist.
The majority of patients make it through the GRTP with no issues at all and return to full sporting activity within the shortest allowed time, however others will take longer between each stage to get back to full activity. Those who remain symptomatic despite prolonged rest will require a review from a sports and exercise medicine consultant or a neurologist.
If a second head injury (which results in a resumption of concussion symptoms) occurs before the full GRTP is completed then the clock will restart from the point of that head injury. It is well known that a second head injury following a concussion (within a few months) is likely to result in more significant symptoms than the first episode and can be fatal in the case of second impact syndrome.
What about Children?
 Children (under 19 are treated differently to adults due to the developmental stage of their brain. Patients 12 years and younger use a specific SCAT 5 designed for children.
Children (under 19 are treated differently to adults due to the developmental stage of their brain. Patients 12 years and younger use a specific SCAT 5 designed for children.
U19’s who have no baseline SCAT’s must wait 2 weeks as a form of rest period before starting the first activity stage on the GRTP. They then have 48 hours between each stage and must be cleared by a doctor at the end regarding return to sport. The earliest they can return to sport would therefore be 23 days
U17-U19’s who have a baseline SCAT and regular doctor contact can shorten their rest period to 7 days before starting the physical activity stages, which have 24 hours between each of them. However they must be reviewed (by a doctor) after the rest period and again at the end of the physical activity stages if they wish to be accelerated in the return to play over a 12-day period.
What examples are the of the GRTP physical activity stages?
 Stage 1 – the rest period (length defined by age and doctor accessibility)
Stage 1 – the rest period (length defined by age and doctor accessibility)
Stage 2 – light aerobic exercise – e.g. walking, riding a stationary bike
Stage 3 – sport specific drills – e.g. running drills, multi directional work but no contact
Stage 4 – non contact training – e.g. hockey practice with no tackling
Stage 5 – contact training – full training involving tacking
Stage 6 – Normal-sporting activities
What advice do you give them to take away?
Those with a diagnosed concussion should not be allowed to drive themselves away, or to continue taking part (if applicable) and so help with transport (and bike storage) may be required.
Patients should also be given head injury advice leaflet, detailing the potential red flags along with a concussion information sheet.
Lastly don’t forget to consider their daily commute – if they cycle or run to work this needs to be reintroduced only at the appropriate GRTP stage.
How can I find out more on this topic?
Feel free to contact us at enquiries@sportsmedicsltd.comand we will be happy to help answer your questions.
Thanks to RFU Headcase and the NHS.
RFU Headcase: Concussion
Headcase: Alternate Link
NHS Conditions: Concussion


